Blog
The MULTI-ACT project is in the final stages of developing a key component of the research and innovation documentation infrastructure to ensure effective and outcome-orientated cooperation between …
Does health research and innovation impact patients? How are we currently measuring this? At present, the impact of research and innovation (R&I) is evaluated primarily through scientific …
Have you ever heard about Patient Reported Outcomes; do you know what they are? Patient Reported Outcomes (PROs) are: “Any outcome evaluated directly by the patient him/herself and based …
What is Theory of Change and why is it a useful, yet imperfect, approach for making change real India, West Bengali. It is a sunny morning and a brand-new project is about to start: it is a …
A central activity in MULTI-ACT is the establishment of a group of experts focused on patient engagement: the Patient Engagement Group (PEG). This PEG has developed guidelines to engage patients …
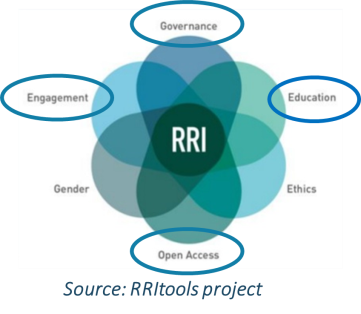
Over the last decade, several attempts have been made to try and reduce the distance between science and society. These have led to the definition of a new approach, which has been called …
